Is it Strep or just a sore throat? Here’s how doctors tell the difference.
So you have a sore throat. Should you just rest and gargle, or schlep to the doctor’s office?
Strep throat, or Streptococcal pharyngitis, is a bacterial infection that can be treated with antibiotics to shorten the duration of symptoms and prevent complications. It’s most common in young, school-age children. When an adult gets a sore throat, 90% of the time it’s caused by a common cold or virus that antibiotics won’t help. But they both feel like crap, so how do you tell the difference?
In health care we use an algorithm called the Centor Criteria to make the call. It’s a clinician’s quick-and-easy way to figure out the likelihood that someone with a sore throat has a bacterial infection that should be treated. It’s not usually used by people outside of the medical profession, and it’s filled with jargon meant for doctors and nurses — but I’ve translated it into plain English for you. You’re welcome. :)
If you come down with a sore throat, take the quiz below, add up your points, and find out what your primary care provider would do next.
Sore Throat Quiz
1) How old are you?
3–14 years old (1 point)
15–44 years old (0 points)
45 years or older (-1 point)
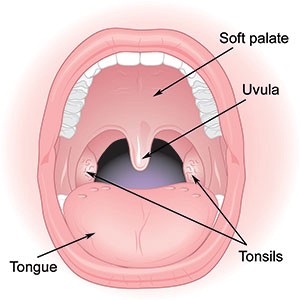
2) Do you have white pus (“exudate” in medical jargon) on your tonsils? (1 point)
Have a friend or family member take a look with a flashlight, or open wide and look in the mirror. I won’t post it here because it’s kind of icky, but if you want to know what pus on your tonsils really looks like, check out this Google Image Search for “tonsillar exudate."
Look for clear spots or streaks of white pus on your tonsils (credit: myclevelandclinic.org).
3) Do you have swollen, tender lymph nodes on the front sides of your neck? (1 point)
Lymph nodes make immune cells. They swell up and can become tender when they’re hard at work making white blood cells to fight infections. When you have an upper respiratory infection (URI), the lymph nodes on either side of your Adam’s apple will be swollen.
4) Do you have a fever? That’s over 100.4°F or 38°C. (1 point)
It’s common to have low, temporary fevers with viral URIs like the common cold. A higher fever that lasts longer than a couple days is more likely to be caused by a bacterial infection like Strep. If you haven’t checked your temperature but you’re pretty sure you have a fever, that counts, too.
5) Do you have a cough? (0 points if yes, 1 point if no)
If you do, it’s much more likely to be caused by a cold virus giving you sinus congestion that’s draining into your throat. You’re more likely to have Strep if you don’t have a cough.
Total up your points
If you got a 3, 4 or 5, you meet Centor Criteria. This doesn’t mean you necessarily have Strep throat, but it does mean you should be tested for Strep in the office. Your provider will either do a Rapid Strep Test or take a swab from your throat for a bacterial culture, or both. The results will indicate whether you have Strep and should be treated.
I made this for you based on the Centor Criteria and the Infectious Disease Society of America’s 2012 guidelines.
Treating Strep Throat
The treatment for Strep throat is penicillin, usually taken for 10 days (ask your provider about alternative antibiotics if you’re allergic to penicillin). Taking an antibiotic for Strep alleviates your symptoms and makes you less contagious. It also lowers your risk of developing a more serious throat infection or a very rare complication called rheumatic fever, which primarily affects the heart and joints.
Here are some reasons you might not want to take antibiotics, even if you have a strep infection:
You’re a healthy adult and you’d prefer to avoid antibiotics. If you rest and drink plenty of fluids, your immune system can actually handle a Strep infection on its own. You’ll get through it more comfortably if you treat your symptoms with the over-the-counter meds suggested below.
You want to avoid common side effects of antibiotics such as upset stomach, diarrhea, and, if you’re a woman, yeast infections. Antibiotics can do quite a number on the helpful bacteria in your body.
If you do start antibiotic treatment, remember to take every single dose of the medication all the way to the end, even if you start feeling better earlier, in order to prevent the bacteria from developing resistance to the antibiotics.
Managing Your Symptoms
Treating your symptoms often doesn’t mean taking antibiotics. Whether your upper respiratory infection is viral like the common cold or bacterial like Strep, the same rules apply for symptom control:
For sore throats, fever, headaches, and body aches: Take acetaminophen (Tylenol) or an anti-inflammatory pain reliever like ibuprofen (Advil, Motrin), naproxen (Aleve), or aspirin as directed. Special note: Never give aspirin to kids under 18 due to the risk of developing Reye’s Syndrome.
For congestion or sinus pressure caused by a head or chest cold: Try steam inhalation, nasal irrigation with a neti pot, over-the-counter nasal steroids like fluticasone (Flonase), or a strong decongestant like real pseudoephedrine (show your ID at the pharmacy counter to get it).
-----
A version of this article was originally published on the One Medical Blog.